How Healthcare Payers Can Leverage CMS Changes to Innovate and Enhance Member Experience

The modern healthcare landscape is always evolving. As payers, you must be skilled at adapting to meet the needs of your members and to ensure timely compliance with shifting regulations.
How are you preparing for the upcoming CMS changes around utilization management and unused supplemental benefits? They’re fast approaching, necessitating payers to make plans to address them sooner rather than later.
While these CMS changes will have implications for data management and scalability, the requirements also present opportunities to enrich your member experience, which is vital to keeping members happy and loyal.
Discover how smarter systems can help you simplify compliance and confidently support your members through CMS’s upcoming changes.
An Overview of CMS Changes in 2026
Here’s what’s included in CMS requirement changes for utilization management and unused supplemental benefits, set to take effect on January 1, 2026.
Changes to Utilization Management
- Prior authorization timeframe requirements
- Standard (non-urgent) prior authorization requests must now be completed within 7 calendar days, except for Qualified Health Plans (QHPs) on Federally Facilitated Exchanges (FFEs), which remain at 15 days.
- Expedited (urgent) prior authorization requests remain at 72 hours, except for Medicaid Fee-for-Service (FFS), which moves from unspecified to 72 hours.
- Provider notice, including the denial reason
- Plans must provide denial reasons to both patients and providers via print, portal, email, phone, or fax.
- Prior authorization metrics
- Payers must publicly post prior authorization data on their websites, including:
- All items and services that require prior authorization
- Percentage of standard and expedited requests approved and denied
- Percentage of standard requests approved after appeal
- Percentage of standard and expedited requests approved after extended decision timeline
- Average and median time from request to decision for both standard and expedited requests
- Payers must publicly post prior authorization data on their websites, including:
These changes will impact the following:
- Medicare Advantage
- State Medicaid
- Medicaid managed care and FFS
- CHIP managed care and FFS
- QHPs on FFEs and FFS
Changes to supplemental benefits notifications
For the first time, Medicare Advantage payers will be required to send mid-year notifications to enrollees who have completely unused supplemental benefits.
This new requirement applies to qualified Medicare Advantage members who have not utilized a supplemental benefit—such as dental, vision, or hearing services—by the middle of the plan year.
Notifications must be sent annually between June 30 and July 31, and the content needs to include what benefits are available, how to access them, and where to find additional information.
Currently, there is no existing requirement for plans to notify members about unused supplemental benefits. This new mandate aims to boost transparency and encourage greater utilization of these valuable services.
Let’s explore why these modifications are important and how they can improve both member experience and health outcomes.
Why These CMS Updates Are Needed
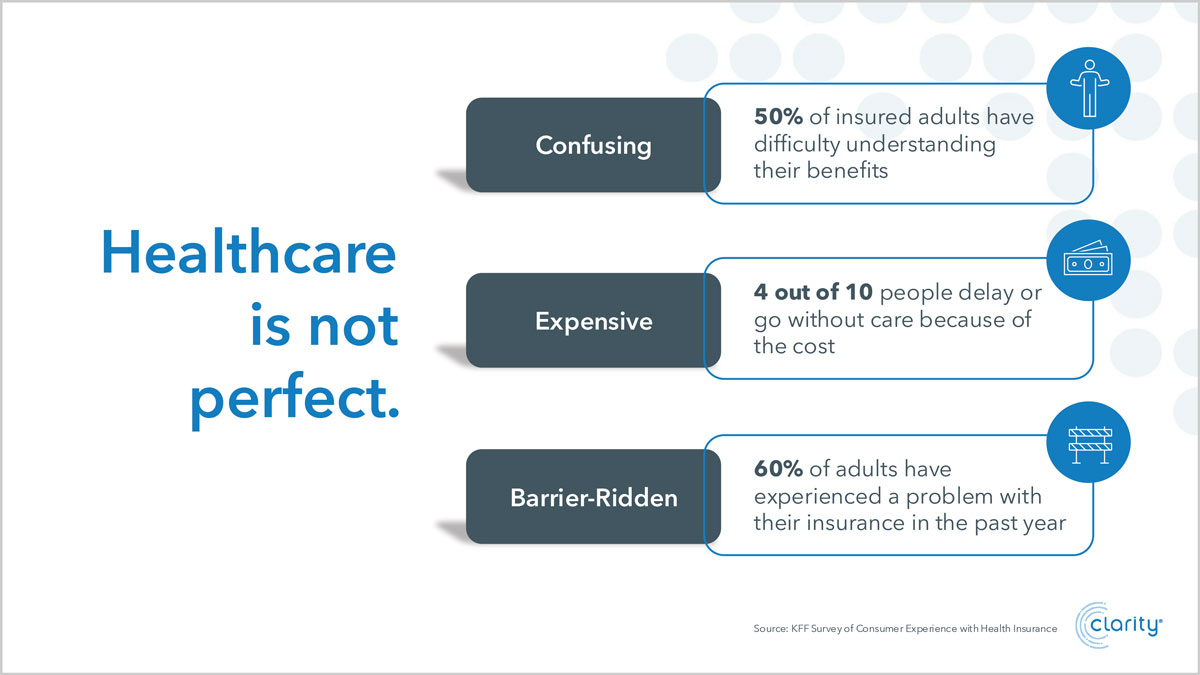
Healthcare can be challenging to navigate.
Benefit confusion is widespread and can lead to real-world health consequences, like care delays and barriers to accessing or affording necessary care.
As a forward-thinking payer, your goal is to help members navigate the system, connect with the care they need, and fully utilize their benefits.
CMS’s upcoming changes can support you in this mission by:
- Elevating the member experience
- Improving equity and outcomes
- Reducing delays and confusion
- Enhancing cost savings
- Refocusing attention on care
Let’s dive deeper into some of the key opportunities these new mandates offer.
Opportunity 1: Elevating the Member Experience
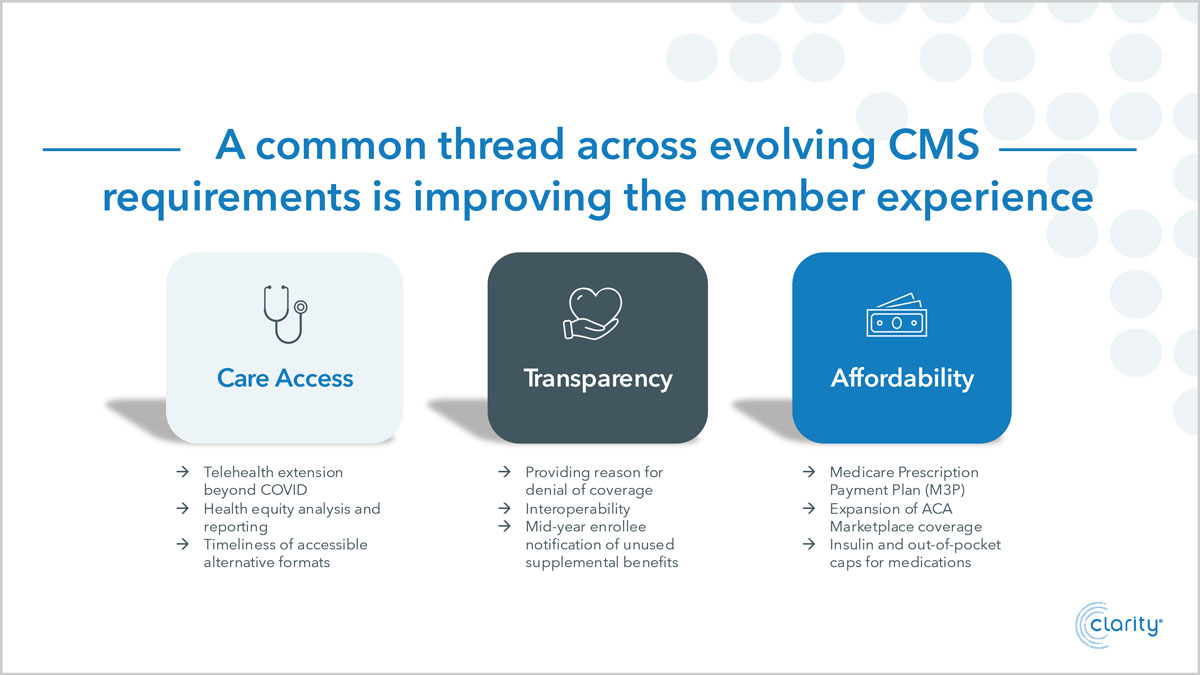
Upcoming changes to utilization management and unused supplemental benefits notifications present payers with a valuable opportunity to enhance the member experience.
Member engagement is crucial to health plan success. Today’s members expect personalized, convenient, and easy-to-navigate experiences.
Yet, issues are rampant:
- 58% of insured adults report problems using their insurance.
- A majority reported issues understanding:
- What their health plan would and wouldn’t cover
- Their explanation of benefits (EOBs) and other communications
- How to find in-network providers
Payers who lean into this moment to create an information-sharing ecosystem can offer their members the support they need.
In a 2022 survey, 22% of adults reported they delayed or did not receive the medical care they needed due to nonfinancial access barriers.
CMS’s changes to utilization management aim to reduce such barriers by enforcing faster turnaround times and heightened transparency with providers and patients.
This helps elevate the member experience in many ways:
- Requiring timely communication of prior authorization denial reasons to both patients and providers helps ensure rapid pivots to alternate care options.
- Improving communication with providers enables them to make informed decisions to help members access their best care options.
- Involving providers facilitates faster appeals, promoting a quicker turnaround.
- Increasing transparency empowers members to assess their plan options based on clear data on which services are approved or denied.
Clear communication is key, and knowledge is power. Sharing the information members and providers need, when they need it, equips them to make the best healthcare decisions.
CMS changes to supplemental benefits notifications also present unique opportunities to enhance the member experience.
A majority of Medicare and Medicare Advantage members report they value their supplemental benefits. Yet, policy differences and coverage confusion often lead to available benefits going untouched.
Upcoming CMS changes address this by requiring Medicare Advantage plans to send an annual communication notifying members of any completely unused supplemental benefits and how to use them.
With this new requirement, payers can be the guide their members often need to navigate their benefits. They can help shine a light on unused supplemental benefits to ensure their members are getting the most from their chosen plans.
Clear, timely communication can also help your members understand how they can best use their benefits to support their health and wellness goals.
Greater awareness leads to greater utilization. Greater utilization leads to better health outcomes. And better health outcomes benefit everyone involved in the healthcare system.
Opportunity 2: Improving Outcomes Through Streamlined Systems

Like healthcare, technology is ever evolving. When leveraged wisely, it’s an empowering tool to support modern healthcare decision-making and utilization.
Savvy payers who invest in multichannel technology will be best equipped as CMS’s changes to utilization management and supplemental benefits notifications take effect.
Opportunities related to utilization management changes
Preventing unnecessary care delays requires fast, effective communication with members and providers.
Information that’s easy to access and understand is vital to achieve this goal. Meet members where they are and guide them to the services they need.
Lead the vanguard by creating thoughtful systems that ensure equitable access to necessary health information. Accelerate information sharing so your members can make decisions quickly with their providers and avoid delays in care.
Your members and their providers deserve to know as soon as possible if and why their prior authorization request is denied. This enables them to file an appeal or pivot to an alternate care plan without delay.
Updated systems allow you to deliver timely, personalized communications that lay out relevant information and options in easy-to-read formats. Members will see you as a trusted partner in their care, who’s there to support and assist them in getting the services they need.
Every touchpoint is an opportunity to strengthen communication and enhance the member experience. Innovative, streamlined systems are the path to this goal.
Leaning into thoughtful design can also help simplify systems for your team. It’s a chance to make healthcare easier and more accessible for everyone.
Opportunities related to supplemental benefits changes
It’s no secret that many healthcare payers face challenges in accurately tracking supplemental benefit usage.
Streamlined, connected systems can help you track how members use their yearly supplemental benefits. This will be essential for providing timely, effective outreach when it’s time to send CMS-mandated notifications. Without that visibility, it’s a last-minute data scramble to figure out which benefits went completely unused at the individual member level.
With enhanced systems that accurately and efficiently monitor compliance and benefit usage, your plan can more easily communicate this information to your members. You can also seize the opportunity to offer personalized guidance on how best to take advantage of their supplemental benefits to support their health and well-being.
Stronger internal processes lead to clearer member communication and greater awareness. When members understand and utilize their supplemental benefits, it drives better access to care and improved health outcomes.
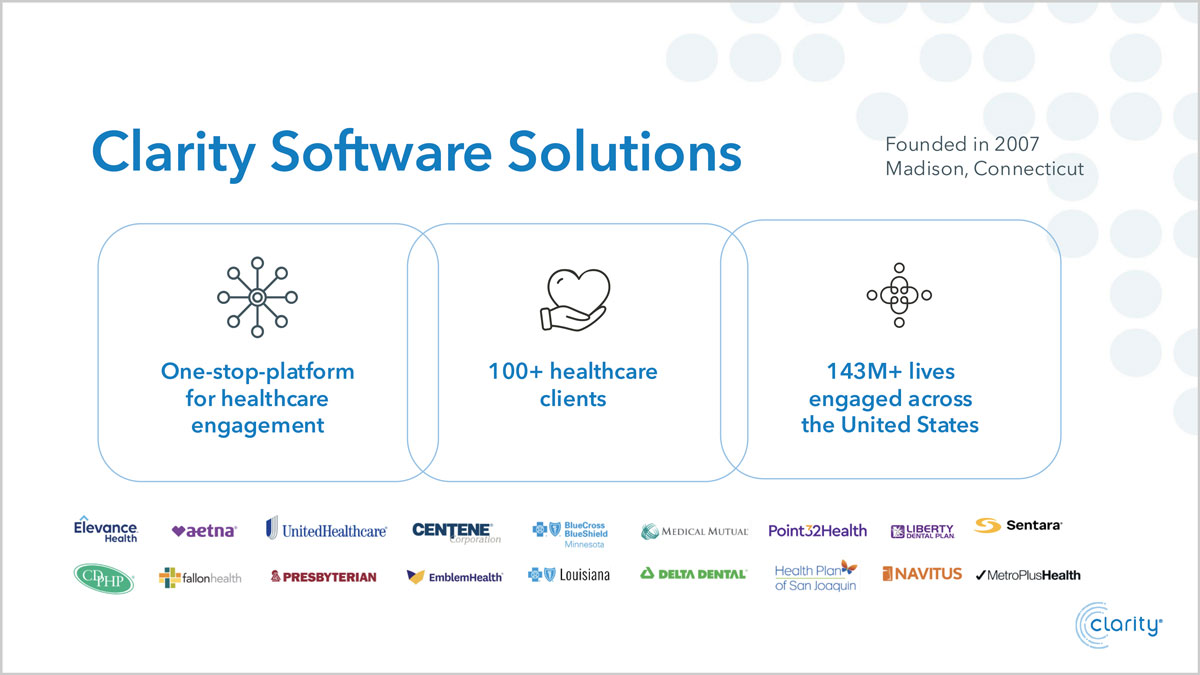
Partner with experts who make healthcare communication clear, compliance easy, and member engagement impactful.
Clarity supports over 100 healthcare organizations across the U.S., helping them meet regulatory requirements while boosting member engagement and satisfaction. We deliver proactive solutions with measurable results for you and your members.
Stay ahead with personalized, multichannel experiences that improve health outcomes and drive meaningful connections. Our transparent communication strategies ensure members receive timely, relevant information in ways they understand.
Simple, accessible messaging not only strengthens your brand, it advances healthcare equity. Clarity helps you meet your members where they are with messages that resonate and inspire action.
Our secure technology transforms complex data into personalized, dynamic designs, backed by innovative tools, guaranteed SLAs, and seamless file management. You’ll meet your deadlines, exceed expectations, and offer members a more trusted, engaging experience that drives results.
Let’s work together to meet CMS requirements and improve healthcare communication for everyone.
Contact us to request a demo or to learn how Clarity can support your goals.
